Sleep Study / Polysomnography (Sleep Study)
Home / Dr. Kushal Chidgupkar
OUR SERVICES
Sleep Study / Polysomnography (Sleep Study)
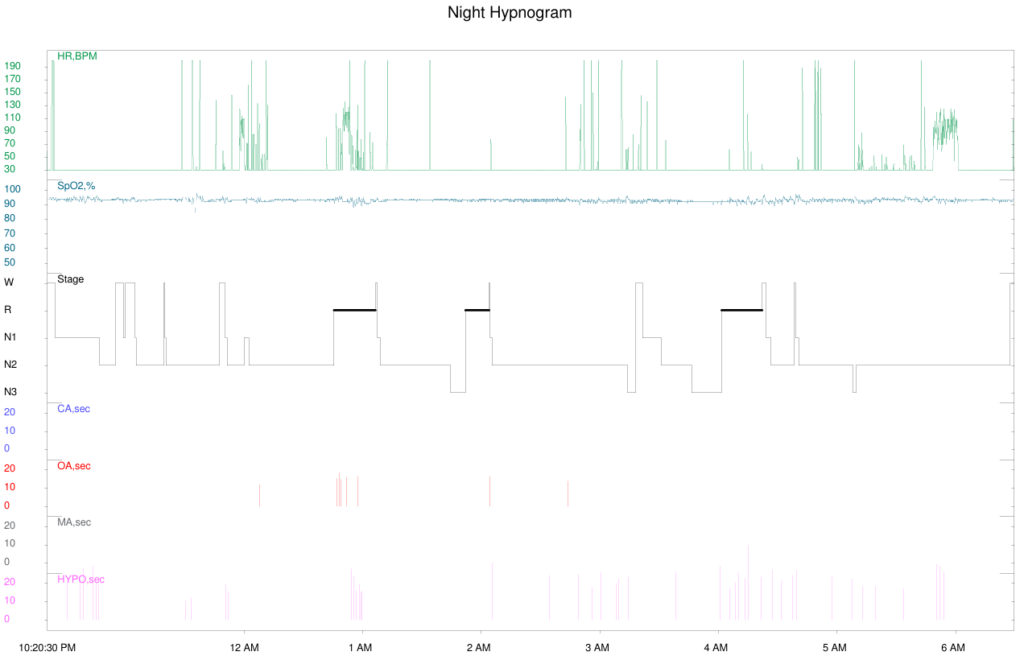
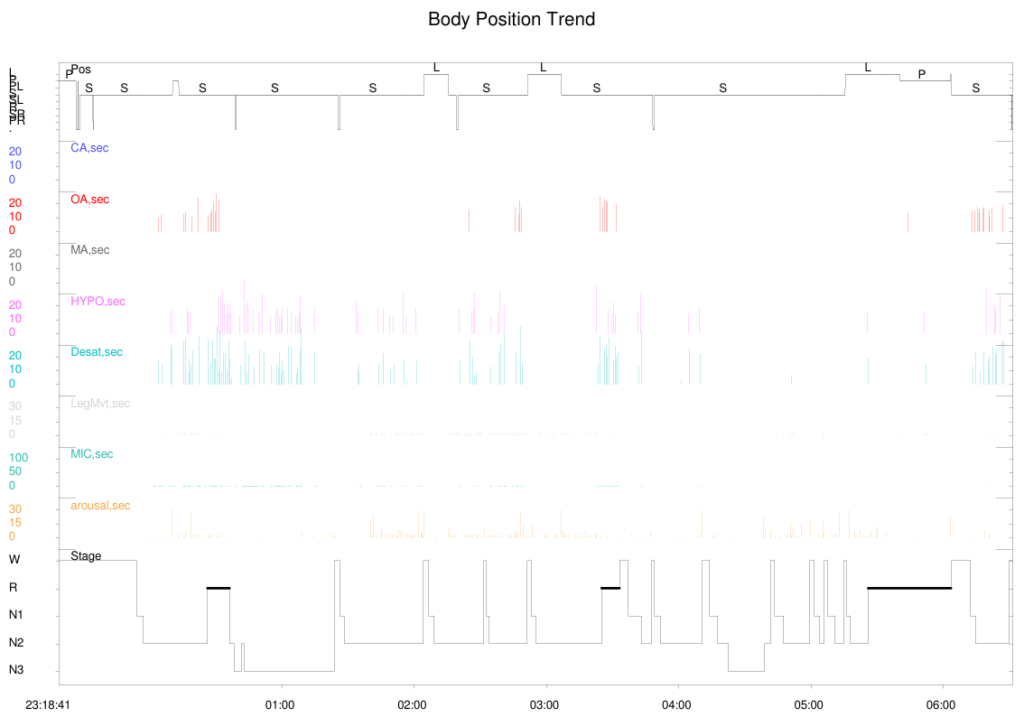
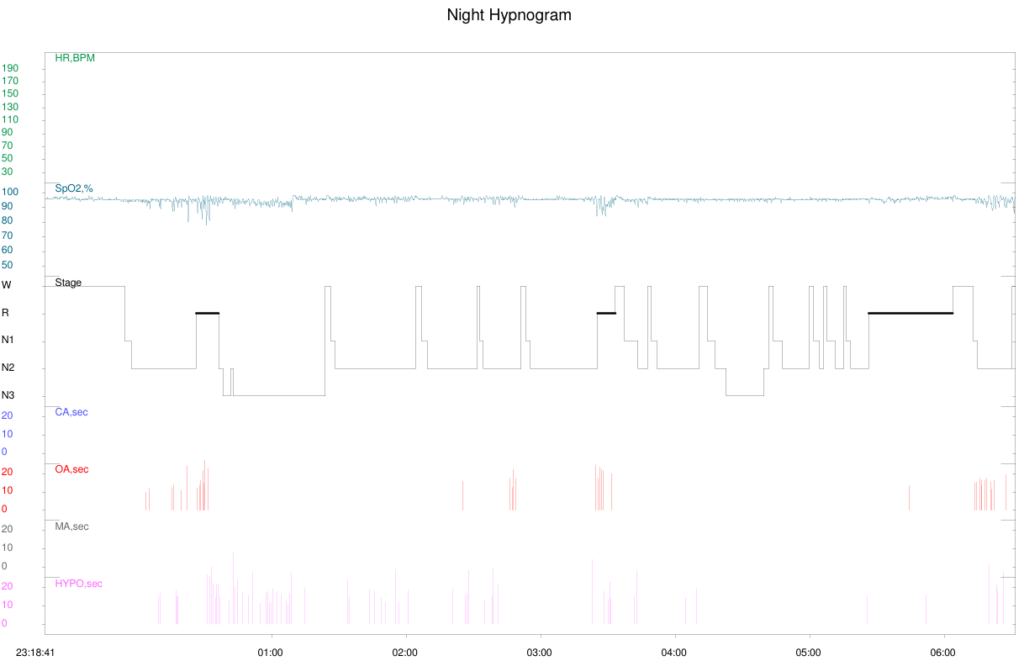
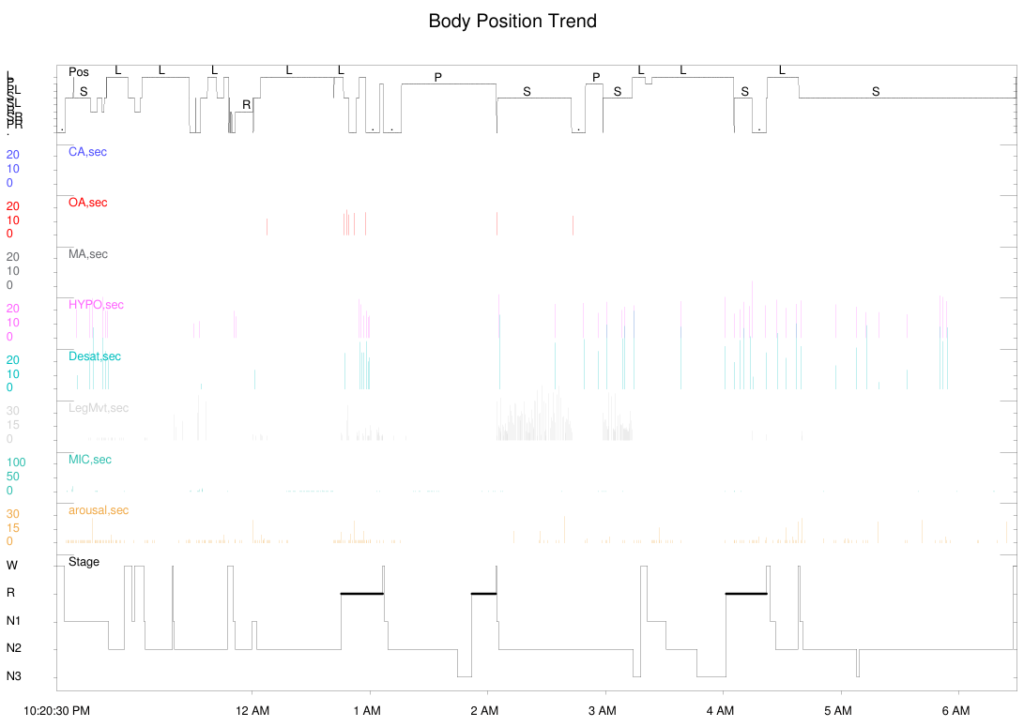
Sleep study also known as Polysomnography, is a test used to diagnose sleep disorders, like Obstructive Sleep Apnea (OSA), Obesity Hypoventilation Syndrome (OHS), Periodic Limb Movement Disorder (PLMD) etc. During this test we record brain waves, oxygen level, heart rate, breathing pattern, body position, chest and abdominal movements, snoring, eye movements and leg movements of the patient during sleep. Sleep study can be done at a sleep lab in the hospital or at the patient’s home. The test is performed at night during sleep. It can also be done during daytime for the shift workers who usually sleep in the daytime. This test involves multiple sensors that track and record all the activities of multiple body systems, including the heart, brain and respiratory system. This gives a comprehensive view of the patient’s sleep quality.
Sleep study is performed in patient who complain of snoring, observed apnea episodes during sleep, disturbed sleep, day time patients sleepiness, fatigue, nocturia, morning headache, forgetfulness, obesity, side neck circumference, neuromuscular disorders, uncontrolled diabetes mellitus, hypothyroidism, or hypertension. It is also performed in patients with history of Myocardial Infection (heart attack), cerebrovascular accident (Stroke), seizure disorder, Parkinson’s disease, as Obstructive Sleep Apnea (OSA) may occur with these conditions.
On the day of sleep study, try to follow usual daily routine. Do not get anxious. Sleep studies are mostly performed at night during the routine sleeping hours of the patient. You can use washroom during the study. On the day of sleep study avoid taking naps in day time, as this can make it harder for you to fall asleep during your sleep study. Avoid caffeine, tobacco and alcohol for at least eight hours before your sleep study. They can disrupt normal sleep pattern and affect the results of sleep study. Wear comfortable clothing during the study.
Sleep Test Details
In sleep study, different sensors are used as the quality of sleep depends on many factors. The number of sensors to be attached depend on the level of the study, and weather the study is performed at home or in the hospital (sleep lab). To achieve a better analysis of sleep, it is recommended to perform level l sleep study in the hospital (sleep lab), where maximum number of sensors are used, Level ll sleep study is performed at Home. Levels lll and IV study should be used to perform follow up studies to assess patient’s progress whenever required. Each of the sensor tracks a specific body system and process, thus enabling deep analysis of the patient’s sleep, which will help in diagnosing certain sleep-related conditions.
A sleep study Involves the following sensors and monitoring methods:-
Electroencephalography (EEG): These sensors have a sticky, electrically conductive gel coating. The coating helps the sensors stick to patient’s head while they detect and record the electrical activity of the brain, known as brain waves, during sleep. Different waves are produced during different stages of sleep. That’s a key way to identify sleep disorders and issues.
Electrocardiography (EKG or ECG): During a sleep study, a single EKG sensor in attached to the chest. This records electrical activity of the heart during sleep. This helps in finding whether there is any issue with your heart’s beating pattern (rhythm) and internal electrical system.
Electromyogram (EMG): These sensors attach to the skin, usually on the face and a leg, to track muscle movement. Unlike a standard EMG, these sensors are used only for monitoring without activating any muscles.
Electro-oculography (EOG): This test involves placing adhesive sensors on the skin around the eyes, Two sensors for each eye as used. These sensors detect eye activities during sleep.
Breathing sensors: These include sensors that detect air movements through the nose and mouth.
Respiratory Inductive Plethysmography (RIP) belt: RIP belt is a device that detects the expansion of the chest and abdomen while breathing during sleep.
Pulse oximeter: This is a small sensor attached to the index finger. It reads the pulse and the oxygen levels in the blood.
Video and audio monitoring: This allows the sleep technician and the specialist to see and hear what is happening during the sleep. It can be used if any of the above sensors give unusual or concerning readings. The recordings are also synchronised with the sensor data, which helps to interpret the sensor reading.
Sleep study can be used in diagnosing the following conditions:-
- Sleep apnea (obstructive and central)
- Obesity Hypoventilation Syndrome
- Periodic limb movement disorder (including restless legs syndrome)
- Insomnia
- Narcolepsy
- Certain types of seizures and epilepsy
- Night terrors (asleep terrors)
- Sleep walking
- REM sleep behaviour disorder and other sleep unexpected behaviour-related disorders
- Nocturnal panic attacks
- Sleep paralysis
- Parasomnias and disruptive sleep disorders
Treatment Approaches
Treatment plans are tailored to the specific sleep disorder and individual needs.
Common interventions include lifestyle and behavioral changes, Cognitive-Behavioral Therapy for insomnia (CBT-I), medications, Continuous Positive Airway Pressure (CPAP) and Bilevel Positive Airway Pressure (BIPAP) for sleep apnea, and other specialized therapies.
Sleep Hygiene
Sleep medicine emphasizes the importance of good sleep hygiene, which includes creating a conducive sleep environment, maintaining a consistent sleep schedule, and adopting habits that promote a restful sleep.
Multidisciplinary Approach
Sleep medicine often involves a collaboration between different healthcare professionals, including pulmonologists, neurologists, psychologists, and otolaryngologists, to provide comprehensive care.
Research and Advancements
Ongoing research in sleep medicine explores the underlying mechanisms of sleep disorders, and also new treatment modalities to improve sleep quality.
Public Health Impact
Sleep disorders can have a significant impact on public health by contributing to conditions such as obesity, cardiovascular diseases, diabetes, hypothyroidism, dyslipidaemia and impaired cognitive function. Sleep medicine professionals work to address these broader health implications.
Telemedicine
Telemedicine has become increasingly relevant in sleep medicine by allowing remote consultations, monitoring, and follow-ups for individuals with sleep disorders.